Rabies - HAN
Jump To:
Overview
Rabies is a disease that is caused by the rabies virus. It affects the nervous system of humans and other mammals. People get rabies from the bite of an animal infected with the rabies virus (a rabid animal).
In the United States, human fatalities associated with rabies occur in people who fail to seek medical assistance, usually because they were unaware of their exposure. The early symptoms of rabies in people are similar to that of many other illnesses, including fever, headache, and general weakness or discomfort. As the disease progresses, more specific symptoms appear and may include insomnia, anxiety, confusion, slight or partial paralysis, excitation, hallucinations, agitation, hyper salivation (increase in saliva), difficulty swallowing, and hydrophobia (fear of water). Death usually occurs within days of the onset of these symptoms. The last human case of rabies in Illinois was reported in 2021.
The vast majority of rabies cases reported in the United States occur in wild animals, like a raccoon, skunk, fox, coyote and bats. Domestic animals such as cattle, cats and dogs account for less than 10% of the reported animal rabies cases.
In Illinois, bats are the primary species identified with rabies. During summer in Chicago, the likelihood of human-bat contact increases because of bat migration and feeding patterns. Although not all bats carry rabies, bats in Chicago and the surrounding area test positive for the virus each year. For Chicago in 2022, the Illinois Department of Public Health tested 165 bats out of which 3 rabies-positive bats were identified.
Rabies in humans is almost always a fatal disease. Therefore, it is critical to provide prompt and appropriate rabies post-exposure prophylaxis (PEP) when bat exposures take place.
Exposures of concern for rabies transmission by bats:
-
If any physical contact with a bat has occurred
-
If an individual awakens and finds a bat in a room or if a bat is seen in the room of a sleeping person
-
If a bat is found in the room of an unattended child
-
If a bat is seen near a mentally impaired or intoxicated person
-
If a bat is found near an unattended pet
-
NOTE: Bats have very small teeth. Therefore, a bite from a bat may not be felt and may leave marks that are not easily seen.
Information for Providers
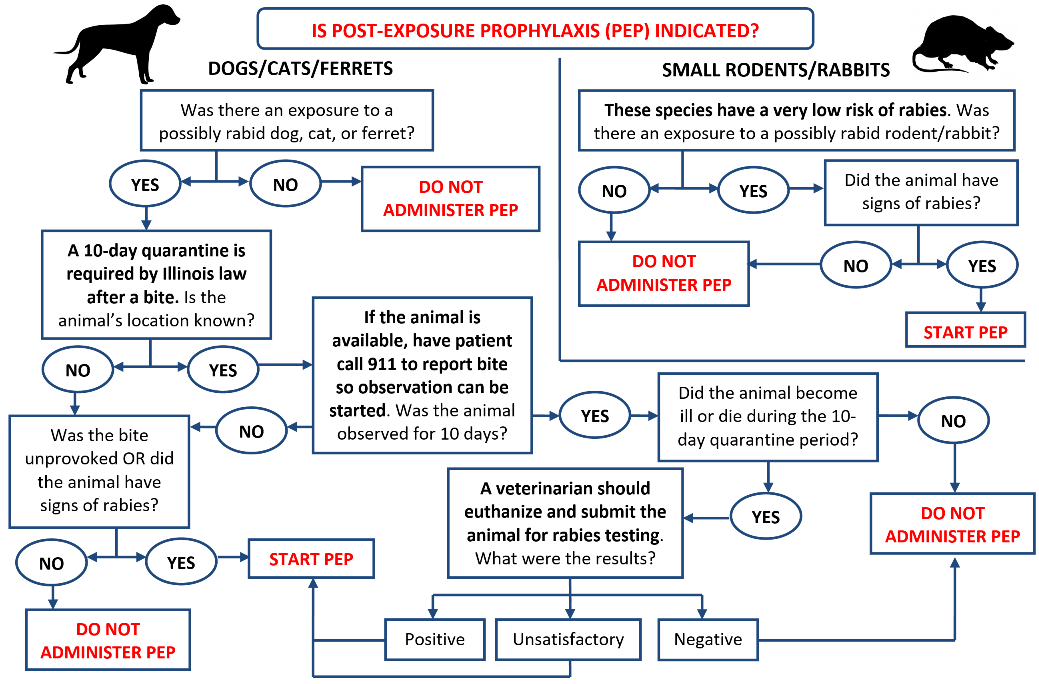
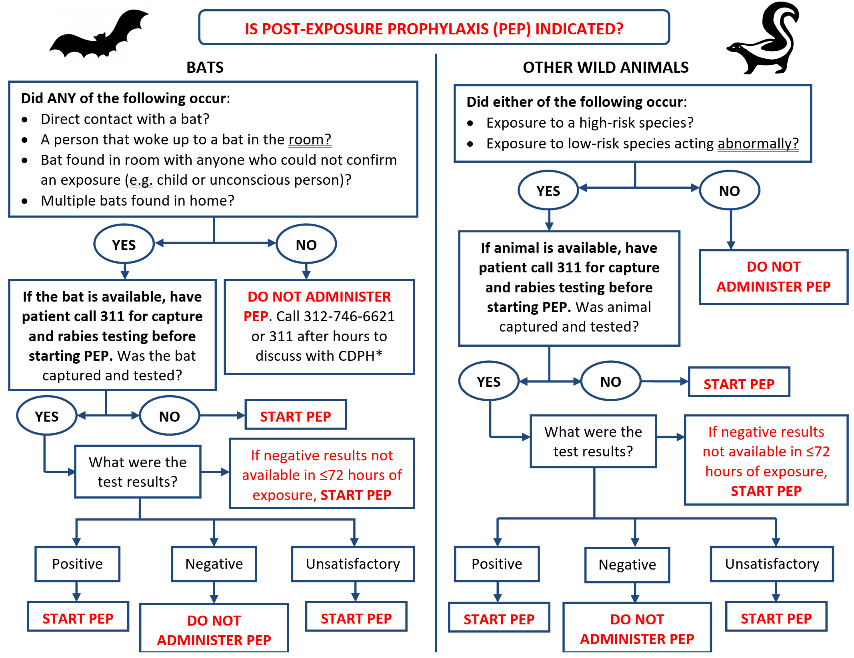
The Chicago Department of Public Health has created an algorithm for providers who are evaluating potential human exposures to rabies for bats & wild animals and domestic animals to help determine whether an individual will require rabies post exposure prophylaxis.
What is a Provoked Bite?
A provoked bite might be expected given the circumstances. Provoked bites can occur when separating two fighting animals, handling an injured or unknown animal, running or biking by a dog, entering a dog's property or taking away an animal's food or toys.
Next Steps After Exposure is Verified
Once the exposure scenario is verified to represent a risk of rabies transmission, the exposed person should receive Rabies Immune Globulin (RIG) and rabies vaccine. The first dose of the 4-dose course should be administered as soon as possible after exposure (day 0). Additional rabies vaccine doses then should be administered on days 3, 7, and 14 after the first vaccination.
Please alert the pharmacy in your facility if you have a potential exposed person to ensure availability if RIG and vaccine.
All individuals receiving post exposure prophylaxis must receive RIG. If your organization does not have access to RIG please contact the health department at 312-743-9000.
Evaluating Potential Human Exposure to Rabies: General
What is a rabies exposure?
Rabies is transmitted through exposure to virus in saliva or brain/nervous system tissue. Rabies exposures can be either:- Bite: Any penetration of the skin, regardless of body site, by the teeth of a potentially rabid animal.
- Non-bite: The contamination of open wounds, abrasions, or mucous membranes (eyes, nose, mouth) with potentially infectious saliva or nervous tissue.
Exposures reportable to CDPH within 24 hours: to report, call 312-743-9000 or 311 if after hours*:
- Any person with exposure to a bat or in the same room as a bat but unaware that direct contact has occurred.
- Any person bitten by a non-human primate or wild mammal, not including small rodents or rabbits.
- Any person started on post-exposure prophylaxis.
- If unsure about PEP, call 312-743-9000, or 311 if after hours, to speak with a Communicable Disease clinician
1
How did the exposure occur?
2
When and where (address, city, state, country) did the exposure occur?
3
What was the animal species? Was it high risk (bat, skunk, racoon, fox, groundhog, non-human primate) or low risk (squirrel, mouse, rat, gerbil, hamster, guinea pig, rabbit, oppossum) species?
4
If low risk species, was the animal acting unusual?
5
Is the animal availble for testing? If so, the patient should call 311 so that the animal may be collected.
Evaluating Potential Human Exposure to Rabies: Domestic Animals
Evaluating Potential Human Exposure to Rabies: Bats and Wild Animals
Rabies Vaccine Information
Summary and Action Items:
- Until further notice, use RabAvert vaccine for rabies vaccination for either pre or post-exposure administration. RabAvert can be purchased directly from the manufacturer on an as-needed basis.
- For rabies immune globulin (RIG), Kedrab and HyperRab are available. Imogam is only available directly from the manufacturer at this time.
- As always, please ensure that persons who are receiving rabies post-exposure prophylaxis (PEP) are recommended for rabies PEP per guidance in the “Human Rabies Prevention-United States, 2008, Recommendations of the ACIP”.
- Correctly administer rabies vaccine to avoid the need to re-do a rabies vaccination.
- Review information on the CDC website.
Background
Imovax (produced by Sanofi Pasteur) is experiencing a temporary supply shortage and is not available at this time. RabAvert vaccine (produced by GlaxoSmithKline) is experiencing a temporary limited supply but is still available for both pre-exposure prophylaxis and PEP. If vaccine is not available from the distributor, order directly from the manufacturer on an as-needed basis. Healthcare providers who are unable to obtain Imovax should use RabAvert during this time, even if Imovax was used to start a pre-exposure or PEP schedule that is in progress.
Both Kedrab (produced by Kedrion Biopharma) and HyperRab (produced by Grifols) are available with no restrictions for rabies immune globulin. Imogam (produced by Sanofi Pasteur) is currently experiencing a temporary shortage. Providers can obtain Imogam directly from the manufacturer.
The CDC continues to work with partners to monitor the status of rabies biologic supplies. The current situation is not expected to impact overall availability of PEP nationally. Healthcare providers should continue to administer PEP when indicated.
For more information please see the IDPH Health Alert issued October 7, 2019.
Rabies Reporting
For Clinical Questions or to Report Suspect Cases, Contact:
The CDPH Disease Reporting Hotline at
312-743-9000
*After hours, weekends, and holidays, call 311 and ask for the communicable disease physician on-call (or 312-744-5000 if outside the City of Chicago).
Reporting also can be done through INEDSS (Illinois Notifiable Electronic Disease Surveillance System) or a Rabies Case Report Form can be completed and faxed back to the Chicago Department of Public Health at 312-746-6388.
Rabies Contacts
CDPH Disease Reporting Hotline
RABIES RESOURCES
| Title | Source | Type |
|---|---|---|
| IDPH Memo: Change in Animal Testing 2016 | IDPH | |
| CDC Rabies Information | CDC | Website |
| IDPH Rabies Information | IDPH | Website |
| MMWR: Human Rabies Prevention | MMWR | |
| MMWR: Updated PEP | MMWR | |
| NASPHV Rabies Compendium | NASPHV | |
| IDPH: Rabies Specimen Euthanasia Requirements | IDPH |
