Acute Flaccid Myelitis (AFM) - HAN
Jump To:
Overview
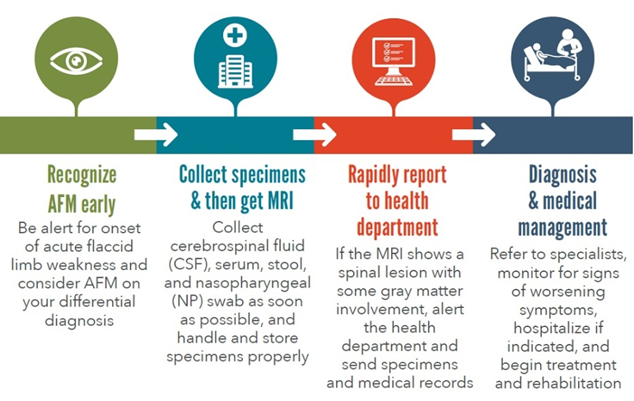
Acute flaccid myelitis (AFM) is an illness characterized by acute onset of flaccid limb weakness and magnetic resonance imaging (MRI) showing lesions in the gray matter of the spinal cord.
About Acute Flaccid Myelitis
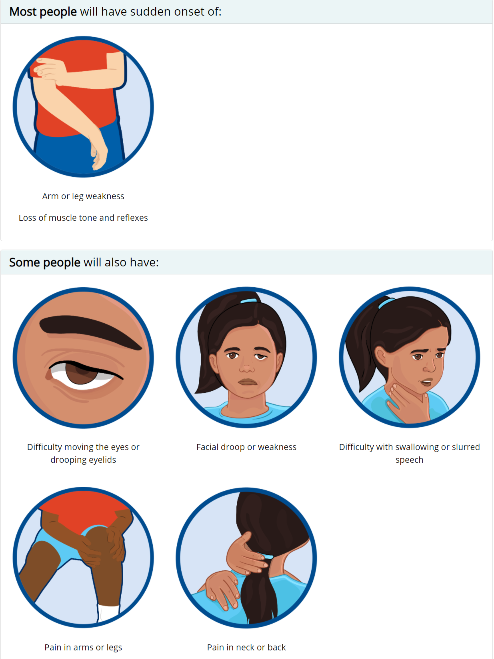
Most AFM cases have arm and/or leg weakness coupled with loss of muscle tone and reflexes. Additionally, some cases have facial/eyelid drooping, difficulty swallowing, slurred speech, difficulty moving their eyes, and/or pain in their arms and legs.
AFM activity peaks in the late summer and early fall and nationwide outbreaks have occurred on a biennial (i.e., every other year) basis since 2014. As of January 3, 2022, there have been 23 confirmed cases in 2021 out of 54 reports of patients under investigation (PUIs) reported to the CDC. Illinois had 0 reported cases in 2021. In 2020 there were 32 confirmed cases out of 59 reports of PUIs. Illinois had 2 reported cases in 2020.
While the cause of AFM has not been identified, it is hypothesized that a viral agent (e.g., enterovirus D68) is involved, as almost all (90%) AFM cases had a preceding respiratory illness and/or fever, increased incidence of AFM cases typically coincides with EV-D68 outbreaks, and viral agents (e.g., EV-D68, EV-A71, Coxsackievirus A16) have been detected in the spinal fluid of a small number of AFM cases.
For more information on acute flaccid myelitis, visit the dedicated CDC and IDPH webpages.
On June 3, 2021, CSTE updated it's position statement. Below is a summary of the updates that were made to the CSTE AFM position statement. Changes include:
-
Adding case ascertainment criteria to allow for the consideration of potential AFM cases identified post mortem
-
Criteria for case ascertainment now includes any person whose death certificate lists AFM as a cause of death or a condition contributing to death
-
-
Adding language to allow for the inclusion of persons with evidence of myelitis on autopsy as AFM cases
-
Criteria for case ascertainment now includes autopsy findings that include histopathologic evidence of inflammation largely involving the anterior horn of the spinal cord
-
Confirmed classification criteria is revised to also include persons who died and did not have an MRI but has evidence of myelitis on autopsy
-
Reporting & Lab Information
AFM Case Definition, 2022
In 2021, the CDC updated the AFM case definition, which is used to ensure consistent and accurate case classification for surveillance purposes. All patients under investigation for AFM will receive final classification by a team of expert neurologists.
Clinical Criteria:
An illness with onset of acute flaccid weakness of one or more limb AND absence of a clear alternative diagnosis attributable to a nationally notifiable condition.
Laboratory Criteria:
Confirmatory laboratory/imaging evidence: MRI showing spinal cord lesion with predominant gray matter involvement and spanning one or more vertebral segment AND excluding lesions caused by physician diagnosed malignancy, vascular disease, or anatomic abnormalities.
Presumptive laboratory/imaging evidence: MRI showing spinal cord lesion where gray matter involvement is present but predominance cannot be determined AND excluding lesions caused by physician diagnosed malignancy, vascular disease, or anatomic abnormalities.
Supportive laboratory/imaging evidence: MRI showing spinal cord lesion in at least some gray matter and spanning one or more vertebral segments, AND excluding persons with gray matter lesions in spinal cord resulting from physician diagnosed malignancy, vascular disease, or anatomic abnormalities.
Case Classification:
-
Confirmed
-
Meets clinical criteria
- Confirmatory laboratory/imaging criteria
- Other criteria:
- Autopsy findings that include histopatholgic evidence of inflammation largely involving anterior horn of spinal cord spanning or more vertebral segments
-
-
Probable
-
Meets clinical criteria
-
Presumptive laboratory/imaging criteria
-
-
Suspect
- Meets clinical criteria
- Supporting laboratory/imaging criteria
- Available information is insufficient to classify case as probable or confirmed
If you have a patient under investigation (PUI) with acute onset of flaccid weakness in one or more limbs:
1
Collect specimens as close to the onset of limb weakness as possible and store according to the table below:
2
Contact the Chicago Department of Public Health (CDPH) via VPD Coordinator Maria Joseph: maria.joseph@cityofchicago.org. You will be provided an authorization number that you will need for specimen submission to the Illinois Department of Public Health (IDPH).
3
Complete the CDC Patient Summary Form (Instructions). Medical records including the MRI report, MRI images, and the neurology consult note will need to be sent to CDPH as well.
MRI Images can be uploaded to: Ambra | Share (ambrahealth.com)
The patient summary form and all medical records can be uploaded via: https://redcap.link/misc_afm.
At the 60 day patient follow-up, additional records will be required if patient has been classified by the CDC as a confirmed or probable case. These include: history and physical, neurology and infectious disease notes, discharge summary, clinical laboratory testing results, and vaccination registry data.
4
Complete the IDPH Communicable Diseases Laboratory Test Requisition Form. On the top of the form, write the authorization number that was provided to you by CDPH. Chose 'Other' for the test and specify 'AFM Study'.
5
Ship specimens, along with the CDC Patient Summary Form, and the IDPH Communicable Disease Laboratory Test Requisition to:
Illinois Department of Public Health Laboratory
Attn: Virology
2121 W. Taylor Street
Chicago, IL 60612
IDPH Lab Contact Phone Number: 312-793-4760
6
Last updated: September 27, 2022
AFM Symptoms
AFM is an uncommon but serious neurologic condition. Sudden onset of arm or leg weakness, loss of muscle tone, and loss of reflexes are the most common symptoms.
Resources - Acute Flaccid Myelitis
Title |
Source |
Type |
|---|---|---|
CDC |
Website
|
|
CDC |
Website
|
|
CDC |
Website
|
|
CDC |
PDF
|
|
CDC |
Website
|
|
IDPH |
Website
|
|
CDC |
Website
|
|
Siegel Rare Neuroimmune Association |
Website |
|
| AFM Presentation | IDPH |
PDF
|
| AFM Resource Library | Siegal Rare Neuroimmune Association |
Website
|
| AFM Task Force | CDC |
Website
|
| Clinical Management of AFM Cases |
CDC
|
Website
|
| Enterovirus D68 Home Page | CDC |
Website
|
| Frequently Asked Questions by Clinicians and Health Departments | CDC |
Website
|
| How to Spot Symptoms of Acute Flaccid Myelitis in Your Child Infographic | CDC | Website |
| List of Reportable Diseases in Illinois | CDPH |
About AFM - Trainings, Webinars, And Notable Publications
Alerts & Communications
AFM Webinar For Clinicians (Dr. Sue Hong, Lurie Children's Hospital, Fall 2020, on behalf of Illinois AFM Learning Collaborative)
Date |
Title |
Source |
Type |
|---|---|---|---|
September 2022 |
CDC HAN: Severe Respiratory Illnesses Associated with Rhinoviruses and/or Enteroviruses Including EV-D68 – Multistate, 2022 | CDC |
|
| September 2022 | IDPH: Health Advisory - Acute Flaccid Myelitis / Polio Virus | IDPH | |
| August 2022 | Update On Poliovirus In The United States - August 26, 2022 | CDPH | Website |
| August 2019 | AFM SIREN Alert | IDPH | |
| May 2019 | AFM Update | CDC | Website |
| September 2018 | CDPH |
AFM Reporting
For Clinical Questions or to Report Suspect Cases:
Complete the Online Case Report FormOR
Call the CDPH Disease Reporting Hotline at 312-743-9000
*After hours, weekends, and holidays, call 311 and ask for the communicable disease physician on-call (or 312-744-5000 if outside the City of Chicago)
When to Report
Clinicians should continue to be vigilant and send information to Chicago Department of Public Health (CDPH) for all patients under investigation (PUI) with sudden onset of neurologic illness associated with limb weakness that meet the case definition for Acute Flaccid Myelitis. Clinicians should send information for PUIs who meet the case definition regardless of any laboratory results.
